Bread; a food most quacks can agree is terrible for you.
Much of the therapeutics I was taught as part of my pharmacy degree is now of historical interest only. New evidence emerges, and clinical practice change. New treatments replace old ones – sometimes because they’re demonstrably better, and sometimes because marketing trumps evidence. The same changes occurs in the over-the-counter section of the pharmacy, but it’s here marketing seems to completely dominate. There continues to be no lack of interest in vitamin supplements, despite a growing body of evidence that suggests either no benefit, or possible harm, with many products. Yet it’s the perception that these products are beneficial seem to be seem to continue to drive sales. Nowhere is this more apparent than in areas where it’s felt medical needs are not being met. I covered one aspect a few weeks ago in a post on IgG food intolerance blood tests which are clinically useless but sold widely. The diagnosis of celiac disease came up in the comments, which merits a more thorough discussion: particularly, the growing fears over gluten consumption. It reminds me of another dietary fad that seems to have peaked and faded: the fear of Candida.
It wasn’t until I left pharmacy school and started speaking with real patients that I learned we are all filled with Candida – yeast. Most chronic diseases could be traced back to Candida, I was told. And it wasn’t just the customers who believed it. One particular pharmacy sold several different kits that purported to eliminate yeast in the body. But these didn’t contain antifungal drugs – most were combinations of laxative and purgatives, combined with psyllium and bentonite clay, all promising to sponge up toxins and Candida and restore you to an Enhanced State of Wellness™. There was a strict diet to be followed, too: No sugar, no bread – anything it was thought the yeast would consume. While you can still find these kits for sale, the enthusiasm for them seems to have waned. Whether consumers have caught on that these kits are useless, or have abandoned them because they don’t actually treat any underlying medical issues, isn’t clear.
The trend (which admittedly is hard to quantify) seems to have shifted, now that there’s a new dietary orthodoxy to question. Yeast is out. The real enemy is gluten: consume it at your own risk. There’s a growing demand for gluten labeling, and food producers are bringing out an expanding array of gluten-free (GF) foods. This is fantastic news for those with celiac disease, an immune reaction to gluten, where total gluten avoidance is essential. Only in the past decade or so has the true prevalence of celiac disease has become clear: about 1 in 100 have the disease. With the more frequent diagnosis of celiac disease, the awareness of gluten, and the harm it can cause to some, has soared. But going gluten free isn’t just for those with celiac disease. Tennis star Novak Djokovic doesn’t have celiac disease, but went on a GF diet. Headlines like “Djokovic switched to gluten-free diet, now he’s unstoppable on court” followed. Among children, there’s the pervasive but unfounded linkage of gluten consumption with autism, popularized by Jenny McCarthy and others. Even in the absence of any undesirable symptoms, gluten is being perceived as something to be avoided.
What’s been lost in an enthusiasm for gluten avoidance, is the fact that there are some people who do experience undesirable symptoms from gluten consumption, but don’t have celiac disease. It’s this group that was the focus of a recent paper in the Annals of Internal Medicine: “Nonceliac Gluten Sensitivity: Sense or Sensibility?” It’s behind a paywall, but I’ll try to summarize the paper in the context of what we know, and what we don’t know, about celiac disease and possible non-celiac gluten sensitivity.
Celiac disease
Celiac disease (CD) is an autoimmune disease, not an allergy or intolerance. The disease manifests with inflammation and injury to the bowel lining when gluten is consumed. It can cause gastrointestinal scarring and villous atrophy – resulting in permanent damage. While it normally presents with gastrointestinal symptoms, symptoms can also manifest as conditions like skin rash.The disease has been described as protean, which is appropriate. A 2001 survey of patients with confirmed celiac disease indicated patients reported symptomatic disease an average of 11 years before a diagnosis was reached. A similar survey of pediatric patients suggested a similar trend: Multiple physicians and other diagnoses. By manifesting in so many different ways, it cannot be diagnosed based on symptoms alone. So why is it so difficult to identify? It isn’t – but you need to look for it.
The immunologic response in celiac disease is a reaction to gliadin, a protein found in wheat, barley and rye. A highly effective test is now widely available. Blood is tested for IgA antibody human recombinant tissue transglutaminase (IgA-tTGA) or endomysium (IgA-EMA). These tests are both highly sensitive (90%–96%) and specific (>95%) for celiac disease. Positive results are followed by biopsy, necessary to establish a diagnosis. That diagnosis is confirmed by evaluating the effectiveness of a gluten-free diet on reported symptoms. (The full diagnostic workup is nicely summarized in the AGA Institute Medical Position Statement on the Diagnosis and Management of Celiac Disease.) Given the availability of a sensitive and specific test for celiac disease, there has been some discussion on whether widespread and routine screening for celiac disease should occur. The evidence and risk/benefit currently suggests screening in the absence of any symptoms is still unwarranted.
Non-celiac gluten sensitivity
We have a sensitive and specific test for celiac disease, so diagnosis should be straightforward, right? If you have celiac disease, you must avoid gluten for life. But what about those that test negative for celiac disease, but have symptoms from eating gluten-containing foods? There are at least five possible scenarios:
- You could be IgA deficient, in which case there’s a false negative. Other laboratory tests may be done, and compared with the biopsy.
- You may already be on a gluten-free diet, which will cause a false negative result.
- It could simply be a false negative laboratory test result (no laboratory test is 100% sensitive and specific).
- There may be some form of subclinical CD present (not yet established as fact, but plausible).
- It may not be celiac disease, and other causes need to be evaluated.
It’s this last category, deemed non-celiac gluten sensitivity (NCGS) which is the subject of the recent Annals paper. Despite the identification of NCGS over 30 years ago, it’s only recently that interest seems to have exploded – I count about 336,000 Google results, but only 10 results in PubMed. Remarkably, the Annals paper points out that the public awareness of NCGS exceeds that of celiac disease [PDF].
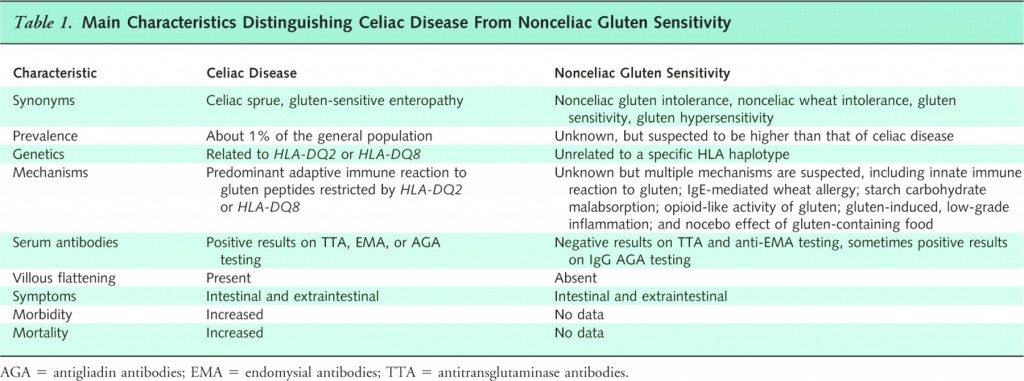
So how do we distinguish between the CD and NCGS, objectively? Here the Annals paper includes a nice table which summarizes the challenge:
It is the protean nature of CD that makes NCGS seem so prevalent. As there’s a myriad of non-specific symptoms that could signal true CD, any any of these symptoms can also be attributed to NCGS. So what high-quality evidence exists to establish NCGS is real? Not a lot, yet. The Annals paper identifies only a single placeb0-controlled rechallenge trial, which concluded that NCGS “may exist”. There is a lack of systematic research, but lots of opinions. A recent essay [PDF] from Sapone et al in Biomed Central used a consensus-based approach to evaluate NCGS and other gluten-related disorders. It concludes by labeling gluten “toxic”, declaring celiac disease an “epidemic”, and suggesting that the prevalence of gluten sensitivity will continue to increase, supposedly because of a lack of adaptive response to deliberate changes bred into wheat strains.
But is that accurate? There are no accurate prevalence estimate for NCGS – because there are no objective signs or symptoms that can be evaluated. Given the magnification of fears of gluten among the general population, I suspect prevalence will increase simply because of perceived health concerns and rank fearmongering over gluten: nocebo effects, where an inert substances causes negative symptoms. From a scientific perspective a few possible mechanisms that have been postulated for NCGS, none of which have been established yet:
- a stress response, rather than an immune response, which is unlikely given the varied manifestations of NCGS
- an IgE-mediated reaction to wheat flour, possibly to another chemical compound it contains
- starch malabsorption
- opioid-like effects of gluten on the colon (opioid receptors in the gastrointestinal tract are the reason narcotics cause constipation)
- some degree of low-grade inflammation, possibly signalling some sort of subclinical CD, presenting in a way that cannot be diagnosed with the current tests
Conclusion: Gluten sensitivity is not well-supported
The idea that gluten sensitivity is real and widespread goes far beyond the current scientific evidence, and the well-established facts of celiac disease. Time will tell if gluten avoidance follows the path of Candida, and other dietary fears and fads that preceded it. But it doesn’t need to. Given the protean nature of CD, symptoms cannot be dismissed as nocebo effects: A CD diagnosis needs to be ruled out before NCGS is even contemplated. Going gluten-free in the absence of a proper medical evaluation may not be directly harmful, but it complicates a diagnosis. Moreover, it can be expensive, and difficult to maintain 100% avoidance – essential with CD, but not established as necessary with NCGS. Besides, who really wants to cut out all gluten-containing products if they don’t need to? Until better diagnostic criteria are established, the N of 1 trial is probably the most science-based (if impractical) approach: single-blind challenges to measure for subjective or objective symptoms. Our challenge in dealing with dietary fads as health professionals is to recognize that some of our patients are suffering, and evaluate them in a science based way: without dismissing the symptoms, and without advocating dietary transformations that may be unnecessary.
Reference
![]()
Di Sabatino A, & Corazza GR (2012). Nonceliac gluten sensitivity: sense or sensibility? Annals of internal medicine, 156 (4), 309-11 PMID: 22351716